Lower back and neck pain are one of the most common reasons to see a doctor. Pain is usually caused by problems with the musculoskeletal system - more pronounced with problems with the spine, including the bones of the spine (vertebrae), the discs and the muscles and ligaments that support them. Sometimes back pain is caused by a condition that does not affect the musculoskeletal system.
Low back pain is more common in older people, affecting more than half of people over 60. This results in significant costs in terms of health care payments, disability benefits and missed hours of work.
The spine (spine) is made up of vertebrae. There are shock absorbing discs between the vertebrae. Discs have a hard outer layer of fibrocartilaginous tissue and a soft, gelatinous inner substance called the nucleus. Each vertebra has two joints behind the discs. These joints are called facet joints. The articular surfaces of one vertebral body rest on the articular surfaces of the other beneath it, forming a joint. The joints, and with them the entire spine, are stabilized by ligaments and muscles, namely:
- Two psoas-iliac muscles that run on either side of the spine
- Two back erector muscles that run the length of the spine behind it
- Many short paravertebral muscles located between the vertebrae
The spinal cord is located in the spinal canal. Along the entire length of the spinal cord, through the holes between the vertebrae on both sides, exit the spinal nerves, the function of which is to unite all the nerves of the body. The part of the spinal nerve near the spinal cord is called the root. Due to the peculiarities of the position of the roots of the spinal nerves, they can be squeezed (compression) with injury to the spine, resulting in pain.
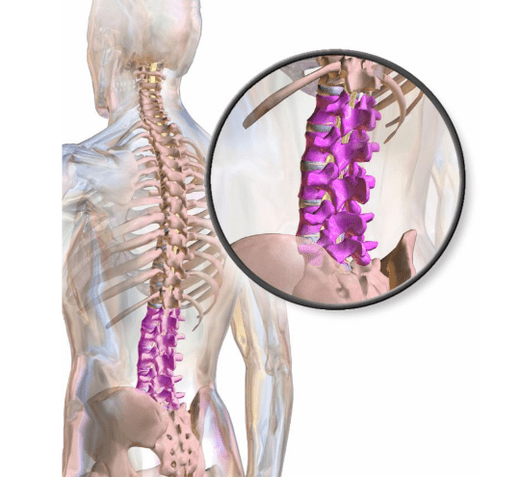
The lower spine (lumbar column) at the top connects to the upper spine (thoracic column) and below the pelvis through the sacrum bone. The lumbar spine is flexible enough to bend, twist, and bend, and provides strength while standing, walking, and lifting. Thus, the lower back is involved in almost all types of daily activities. Low back pain can interfere with various activities and worsen quality of life.
Types of back pain
Common types of low back pain include localized, radiating, and repercussion pain.
Local painappears in a certain area of the lower back. It is the most common type of back pain. The cause is usually disc injury, arthritis of the joint and, less commonly, muscle strain. The pain may be continuous and painful, or at some point, it may be replaced by sharp, intermittent pain. Sudden pain can appear when trauma is the cause. Local pain may increase or decrease with a change in position. Touching the lower back can be painful. Muscle spasms are possible.

Radiating painIt is low back pain that extends to the leg. The pain can be dull or sharp and intense. Typically, it affects only the side or back of the leg and can extend to the foot or just the knee. Radiating pain is usually a manifestation of compression of the nerve root of the spine in conditions such as herniated disc, sciatica, osteoarthritis, or spinal stenosis. Coughing, sneezing, straining, or bending over with your legs straight can be painful. When a spinal nerve root is compressed, the pain may be accompanied by weakness in the muscles of the legs, a tingling sensation, or even loss of sensation. In rare cases, loss of control of urination (urinary incontinence) or loss of control of stool (fecal incontinence) occurs.
Thoughtful painfelt in a location other than the actual cause of the pain. For example, some people who have a heart attack experience pain in their left arm. The pain reflected from the internal organs of the lower back is mainly of a deep and painful nature, and its exact location is difficult to determine. As a rule, with movement, the pain does not increase, unlike the pain accompanying disorders of the musculoskeletal system.
The reasons
In most cases, back pain is a consequence of diseases of the spine and surrounding joints, muscles, ligaments and roots of the spinal nerves, as well as the intervertebral discs. Often a single specific cause cannot be identified. Any painful disease of the spine can cause the muscles around the spine to contract reflexively (spasm). The spasm can increase the pain. Stress can make lower back pain worse, but the mechanism is not clear.
Sometimes back pain is caused by a disorder that does not affect the spine, such as cancer, gynecological conditions (such as PMS), kidney disease (such as kidney stones), urinary tract disease (such as infections of the kidneys, bladder, and prostate) and digestive tract (eg, diverticulitis), as well as diseases of the large arteries near the spine.
Common causes
Common causes of back pain are:
- Osteoarthritis
- Compression fractures of the spine
- A ruptured or herniated disc
- Spinal stenosis in the lumbar spine
- Spondylolisthesis
- Damage to muscles and ligaments
- Fibromyalgia
To damagemay occur during normal activities (for example, lifting heavy objects, exercising, unexpected movement) or as a result of an injury, such as a fall or a traffic accident. Usually, imaging studies show no specific lesions, but doctors suspect that certain muscles and / or ligaments are affected.
Osteoarthritis(degenerative arthritis) causes wear and tear of the cartilage between the joint surfaces and the formation of bone spines (osteophytes). This disease is in part the result of years of tissue wear and tear. In severe degeneration and loss of disc height, osteophytes in the foramen can compress the roots of the spinal nerves. All of these changes can lead to lower back pain as well as stiffness.
Compression fractures of the spine (due to compression)(vertebral fractures) often occur when bone density decreases due to osteoporosis, which usually develops with age. However, fractures from osteoporosis tend to occur in the upper and middle back and are accompanied by pain in these areas rather than in the lower spine.
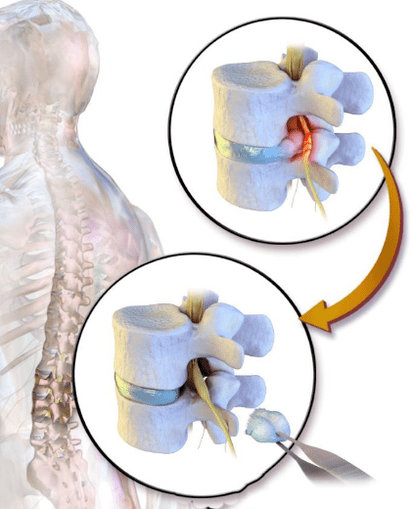
A ruptured or herniated disccan cause back pain. The disc is represented by a dense outer layer and a soft, gelatinous central part. If the disc is under constant stress from the vertebrae above and below (for example, when leaning forward, especially when lifting heavy objects), its outer layer may rupture (tear), causing pain.
Spinal stenosis in the lumbar spine- Narrowing of the spinal canal (which runs through the center of the spine and contains the spinal cord and the bundle of nerves that extend downward from the lower part of the spinal cord) in the lumbar region. It is a common cause of low back pain in the elderly. Spinal stenosis also develops in middle age in people whose spinal canal is narrow from birth. Spinal stenosis is caused by disorders such as osteoarthritis, spondylolisthesis, ankylosing spondylitis, and Paget's disease.
Spinal stenosis can cause sciatica as well as back pain.
Spondylolisthesis- partial displacement of the vertebra in the lower part of the spine. One type usually occurs during adolescence or adolescence (often in athletes) and is caused by an injury that fractures part of the vertebrae. If both sides of the vertebra are affected, the vertebra may slide forward over the underlying vertebra. Spondylolisthesis can also occur in older people, but mainly as a result of degenerative disease. With the development of spondylolisthesis in adulthood, the risk of spinal stenosis in the lumbar region increases.
FibromyalgiaIs a common cause of pain that affects many parts of the body, including the lower back. This condition results in chronic diffuse pain in the muscles and other soft tissues outside of the lower back. Fibromyalgia is also characterized by sleep disturbances and fatigue.
Surveys
Tests are usually not ordered because most back pain is due to osteoarthritis, sprains, or other minor musculoskeletal disorders and goes away within 6 weeks. Imaging tests are often needed if:
- another reason is suspected;
- there are warning signs;
- back pain persists.
An evaluation may also be ordered if there is no response to initial treatment, or if symptoms worsen or change.
X-rays of the lower back can only provide a picture of the bones. Such images can detect degenerative changes due to osteoarthritis, vertebral compression fractures, spondylolisthesis, and ankylosing spondylitis. However, magnetic resonance imaging (MRI) or computed tomography (CT) can provide a clear picture of the bones and, as is typical for MRI, display soft tissue (including discs and some nerves). An MRI or CT scan is usually needed when doctors determine the presence of disorders that lead to certain changes in bone structure, as well as soft tissue disease.
If spinal cord compression is suspected, an MRI is done as soon as possible. In rare cases, when MRI results are ambiguous, it becomes necessary to perform myelography with CT. Rarely, if a malignant tumor or infection is suspected, a tissue sample (biopsy) should be taken for analysis. In some cases, electromyography and exams to study nerve conduction are done to confirm the presence, location, and in some cases the duration and severity of spinal nerve root compression.
Prophylaxis
People can reduce their risk of developing lower back pain by taking the following steps:
- physical exercises;
- exercises to strengthen and stretch the muscles;
- maintain normal body weight;
- maintain correct posture;
- adherence to recommendations for safe weight lifting.
The most effective way to prevent lower back pain is to exercise regularly. Aerobic exercises and special exercises for building muscle strength and stretching are recommended.
Aerobic exercise, such as swimming and walking, improves overall fitness and strengthens muscles.
Special exercises for the development of muscle strength and the stretching of the muscles of the abdominal wall, buttocks and back (deep trunk muscles), stabilize the spine and reduce the stretching of the discs that absorb the muscle. spine and the ligaments that hold them.
Muscle strengthening exercises include pelvic tilts and abdominals. Stretching exercises include stretching by bending the knees towards the chest. In some people, stretching exercises can lead to increased back pain, so caution should be exercised. The rule of thumb is that any exercise that causes or worsens back pain should be stopped. The exercises should be repeated until mild (but not extreme) muscle fatigue is felt. Breathing is essential during exercise. People with back pain should consult a doctor before exercising.
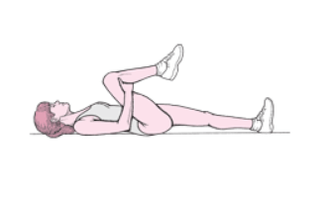
Pelvis tilt
Take a supine position on your back with the knees bent, heels on the floor, load on the heels. Press your back against the floor, squeeze your glutes (lift them about half an inch off the floor), and contract your abdominal muscles. Hold this position for a count of 10. Repeat 20 times.

Cracks of lies
Lie down on your sleep with your knees bent and your feet flat on the floor. Fold your arms over your chest. Tighten your abdominal muscles, slowly lift your shoulders about 10 inches off the floor, keeping your head straight (your chin should not touch your chest). Relax your abdominal muscles, slowly lower your shoulders. Do 3 sets of 10 repetitions.

Stretches with knees to chest
Take a lying position, straighten up. Place both palms under one knee and press it against your chest. Hold for a count of 10. Slowly lower your leg and repeat the exercise on the other leg. Do the exercise 10 times.
Exercise also makes it easier to maintain your desired body weight. Exercise also helps maintain bone density. Thus, exercise can reduce the risk of developing two conditions that can cause lower back pain: obesity and osteoporosis.
Correct posture when standing and sitting reduces stress on the back. Sagging should be avoided. Chair seats should be adjusted in height so that the feet are flat on the floor, the knees slightly bent and the lower back firmly against the back of the chair. If the chair does not support the lower back, a pillow can be placed underneath. When seated, it is recommended to put your feet on the ground and not to cross your legs. Sick people should not stand or sit for long periods of time. If you have to stand or sit for a long time, frequent changes in position can reduce the strain on your back.
Treatment
If it is possible to determine a specific cause, the disease is treated. For example, antibiotics are used to treat an infection of the prostate. However, there is no cure for painful sprains of the musculoskeletal system or pain caused by other conditions. However, the situation can be improved by general measures. As a rule, such measures are also used when compressing the nerve root of the spine.
General measures for back pain
Possible actions include:
- Make changes to activities
- Take pain relievers
- Apply heat or cold to the painful area
- Light exercise, if tolerated
For newer back pain, treatment begins by eliminating activities that strain the back and cause pain, such as lifting weights and bending over. Bed rest does not speed up pain relief, and most professionals recommend doing light work. Bed rest, necessary to relieve severe pain, should not last more than 1 or 2 days. Prolonged bed rest weakens the core muscles and increases stiffness, which worsens back pain and slows recovery. Corsets and traction are ineffective. Traction can slow healing.
Over-the-counter or prescription nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Opioid pain relievers are sometimes prescribed if NSAIDs do not provide sufficient pain relief, but they should only be used for a short time, as long-term use of opioid pain relievers may, conversely, increase sensitivity to pain. pain, cause side effects and increase risk. addiction and dependence.
Muscle relaxants can sometimes relieve muscle spasms, but their effectiveness is questionable. These drugs are not recommended for older patients who are more likely to develop side effects such as drowsiness and disorientation. Doctors try not to prescribe muscle relaxants if the patient does not have visible and palpable muscle spasms. If muscle relaxants are prescribed, they should not be used for more than 72 hours. Doctors sometimes recommend taking them right before bed.
Massage can provide temporary relief from lower back pain. Some studies have shown positive results with acupuncture, others have contradicted these results. Manipulation of the spine by chiropractors or other doctors (such as osteopathic doctors), combined with an exercise program, can also provide pain relief. However, manipulation of the spine can increase the risk of further injury and should be avoided in people with inflammatory arthritis, neck problems that cause cervical instability, or a herniated disc.
It is recommended that you sleep in a comfortable position on a medium firm mattress. People who sleep on their backs should have a pillow under the knees. Patients who sleep on their side should use a pillow that keeps their head in a neutral position (without bending the neck up or down). Patients should place a second pillow between the knees, with the knees and hips slightly bent, if it relieves lower back pain. Patients can still sleep on their stomach if they feel comfortable.
Continue or start taking other preventive measures (correct posture, good weight training technique). With the realization of such events, the back pain attacks mostly disappear within the period of several days to 2 weeks. Regardless of the treatment, 80 to 90% of these attacks resolve within 6 weeks.
Treatment of chronic low back pain
Additional measures are needed to treat chronic low back pain. Aerobic exercise is advised and weight loss is recommended if necessary. If analgesics are ineffective, other treatments should be prescribed.
Transcutaneous electroneurostimulation (TENS) is possible. CHENS devices generate a weak alternating current which causes a slight tingling sensation. This current can block the transmission of certain painful sensations from the spinal cord to the brain. The current can be applied to the painful area several times a day, the duration of the session varies from 20 minutes to several hours, depending on the intensity of the pain.
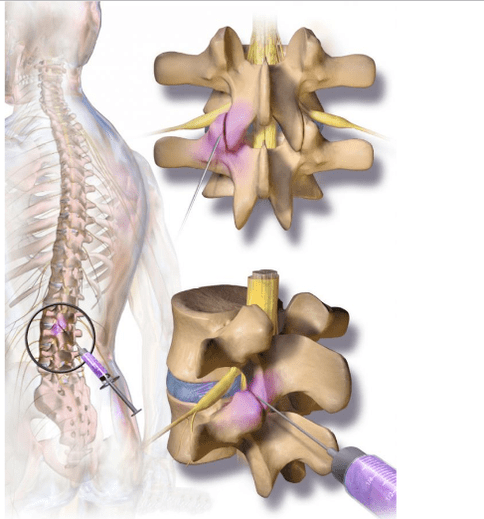
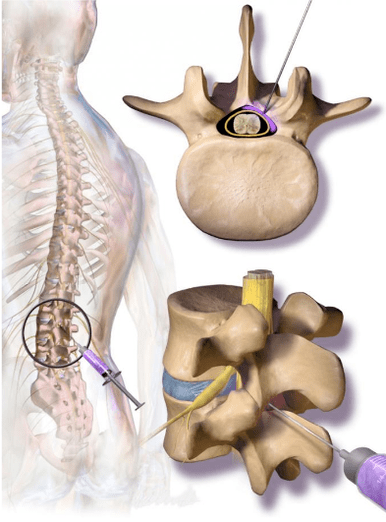
Sometimes corticosteroids with a local anesthetic are periodically injected into the facet joint of the spine or into the epidural space - between the spine and the outer layer of tissue covering the spinal cord. Epidural injections may be more effective for sciatica, which is due more to a herniated disc than to lumbar spinal stenosis. However, they may not have long-term beneficial effects. They usually only last a few days or weeks. Their main goal is to relieve pain so that you can exercise for long term pain relief.
Back pain surgery
In cases where a herniated disc results in persistent or chronic sciatica, weakness, loss of sensation, or fecal and urinary incontinence, it may be necessary to surgically remove the protruding part of the disc (discectomy) and, in some cases, part of the vertebra (laminectomy).
In severe spinal stenosis, a large part of the posterior vertebra (lamellae of the vertebral arch) may be removed to widen it (lumbar laminectomy). General anesthesia is usually necessary. The duration of hospitalization is generally 4 to 5 days. Patients will be able to resume their normal activities in 3 to 4 months. Adequate or complete recovery is observed in approximately two-thirds of patients. For the rest of the patients, such surgery can prevent pain and other symptoms from worsening.
If the spine is unstable (which can result from a severe herniated disc, spondylolisthesis, or laminectomy for spinal stenosis), surgery may be done to fuse the vertebrae (called arthrodesis of the lumbar vertebrae). However, the fusion restricts mobility, can be accompanied by excessive mechanical stress on the rest of the spine and cause problems in the future.
Compression fractures of the spine
Compression fractures of the spine are quite common in women over 50. They can be treated conservatively without surgery, with braces, pain relievers, and possibly calcitonin nasal spray, which will not help bone healing but may reduce pain.
If sufficient pain control cannot be achieved, two surgical options are available:
- Vertebroplasty: injection of cement mortar into a fractured bone.
- Kyphoplasty: Insertion of a balloon into a fractured bone to create space. The balloon is then filled with cement.
However, recent studies have shown that in the long term, the effectiveness of these surgeries does not outweigh the effectiveness of non-surgical treatment options.
Key points
- Low back pain is common. It is usually caused by musculoskeletal disorders of the spine and factors such as fatigue, obesity and insufficient physical activity.
- Low back pain is rarely severe at a young age, and testing is usually unnecessary unless symptoms persist for several weeks.
- Patients with warning signs or patients over 55 years of age should see a doctor immediately.
- Strengthening the muscles of the abdominal wall and back with specific exercises helps prevent the most common types of low back pain.
- For back pain, most often sufficient treatment is to exclude measures with mechanical effects on the back, take pain relievers, and in some cases apply a cold or hot compress.
- Prolonged bed rest and stretching can slow recovery.
- In severe cases, such as abnormal sensations and weakness in the legs, surgery may be necessary.
- Compression fractures of the vertebrae can be treated conservatively (with braces, pain relievers and a nasal spray) or, in some cases, more aggressively with surgery.



































